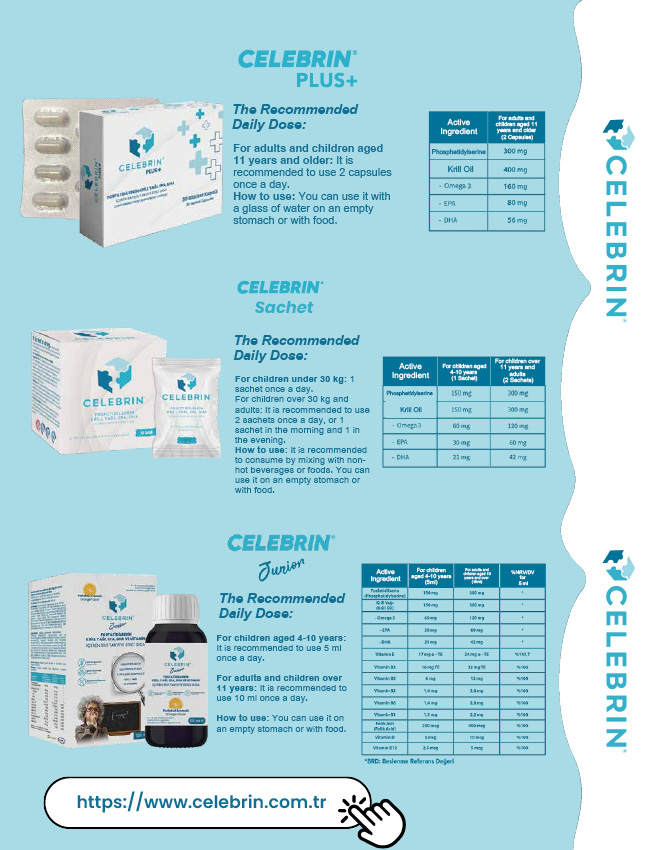
Pneumonia
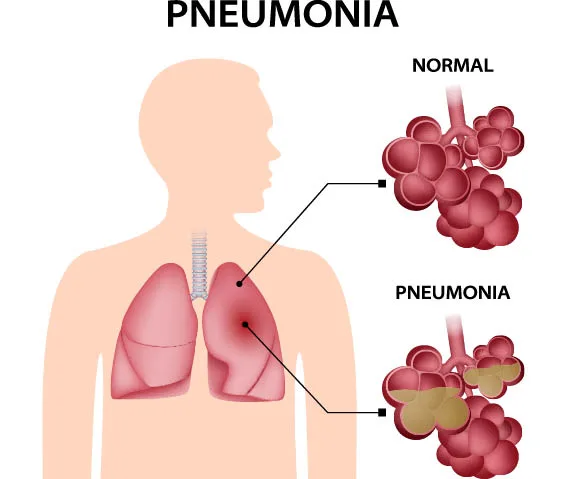
During the winter months, the frequency of respiratory system infections is quite high. Patients with fever and cough who visit the internal medicine clinic are most afraid of the possibility of pneumonia. The same fear is even greater in families with children experiencing fever. Pneumonia, medically known as pneumonia, is the inflammation of lung tissue caused by a variety of microorganisms such as viruses, bacteria, or fungi.
How does Pneumonia spread?
There is a possibility of pneumonia-causing microbes spreading from an infected person to a healthy one. However, the disease often occurs through microbes reaching the lungs from the patient’s throat, mouth, nose, or digestive system. The ability of an infection from a different part of your body to reach your lungs may be influenced by a compromised immune system. Respiratory infections or those transmitted through utensils, such as spoons, forks, glasses, from person to person, like the flu (influenza), COVID, are common starting points for the disease. Factors such as the age of the infected person, smoking habits, existing chronic conditions, and nutrition play a role in determining an individual’s resistance.
Patients who come in for examination often request immune-boosting supplements to avoid getting sick. However, the only true way to prevent getting sick is to protect yourself from the transmission of the actual infection or, if available, getting vaccinated. Once an infection is contracted, the likelihood of it progressing to pneumonia is determined by the effectiveness of your immune system.
Pneumonia is one of the most common causes of death worldwide and in our country.
It ranks as the 5th leading cause of death in our country. Pneumonia can start in different ways. Sometimes, it begins with symptoms like a fever above 38 degrees Celsius, cough, dirty yellow-green phlegm, and chest pain. Other times, it may start with chronic cough, shortness of breath, loss of appetite, and fatigue. In some cases, it can begin with symptoms such as nausea, abdominal pain, and impaired consciousness. The clinical presentation can vary depending on the type of microorganism causing the infection, the affected area of the lungs, the patient’s age, and additional health problems.
When to Consult a Doctor?
In the case of an upper respiratory tract infection, it is advisable to seek medical attention if the fever is above 38 degrees Celsius and persists for 48 hours, if cough and phlegm intensify, and if symptoms such as shortness of breath and loss of appetite arise. However, a deterioration in the overall condition of elderly patients alone necessitates a visit to the doctor. The diagnosis of the illness is typically made by the doctor through patient consultation, examination, determination of infection levels in the blood, and, if necessary, imaging tests such as chest X-rays or CT scans.
The patient’s overall condition, the extent of lung involvement, and any additional health problems are taken into consideration when planning whether the patient should be treated in the hospital or at home. The recovery from the illness often takes around two weeks, but in some cases, it may take longer. Early diagnosis and prompt initiation of treatment yield favorable results, but in cases where the disease is diagnosed late, the process can be challenging enough to require intensive care.
Is it Possible to Prevent Pneumonia?
First and foremost, to prevent upper respiratory tract infections, especially those that pave the way for diseases like the flu and COVID, it is essential to adhere to hygiene practices, mask usage, and vaccination recommendations. To strengthen the immune system, one should avoid smoking and alcohol consumption, adopt healthy eating habits, and ensure adequate rest. Individuals with additional health conditions such as diabetes or heart disease should undergo regular check-ups, maintain good health, and get vaccinated against pneumonia. For those with neurological diseases, special precautions should be taken during meals to prevent food aspiration into the lungs.
Pneumonia Vaccines
There are two types of pneumonia vaccines available worldwide and in our country: conjugate pneumococcal vaccine and polysaccharide pneumococcal vaccine. Both vaccines provide protective effects against Streptococcus pneumoniae, which accounts for 60% of community-acquired pneumonias. They not only protect against pneumonia but also provide immunity against infections such as sinusitis, middle ear infections, and bronchitis caused by this pathogen. In the adult population, vaccination is administered based on risk groups and age. There are vaccination schedules involving the consecutive use of both vaccines, as the streptococcus pneumonia type targeted by the two vaccines and their ability to stimulate immunity differ from each other.
Cicidoktorum says…
If you are 65 years or older, have COPD, heart failure, diabetes, chronic kidney failure, or a suppressed immune system, it is essential to get the pneumonia vaccine.”